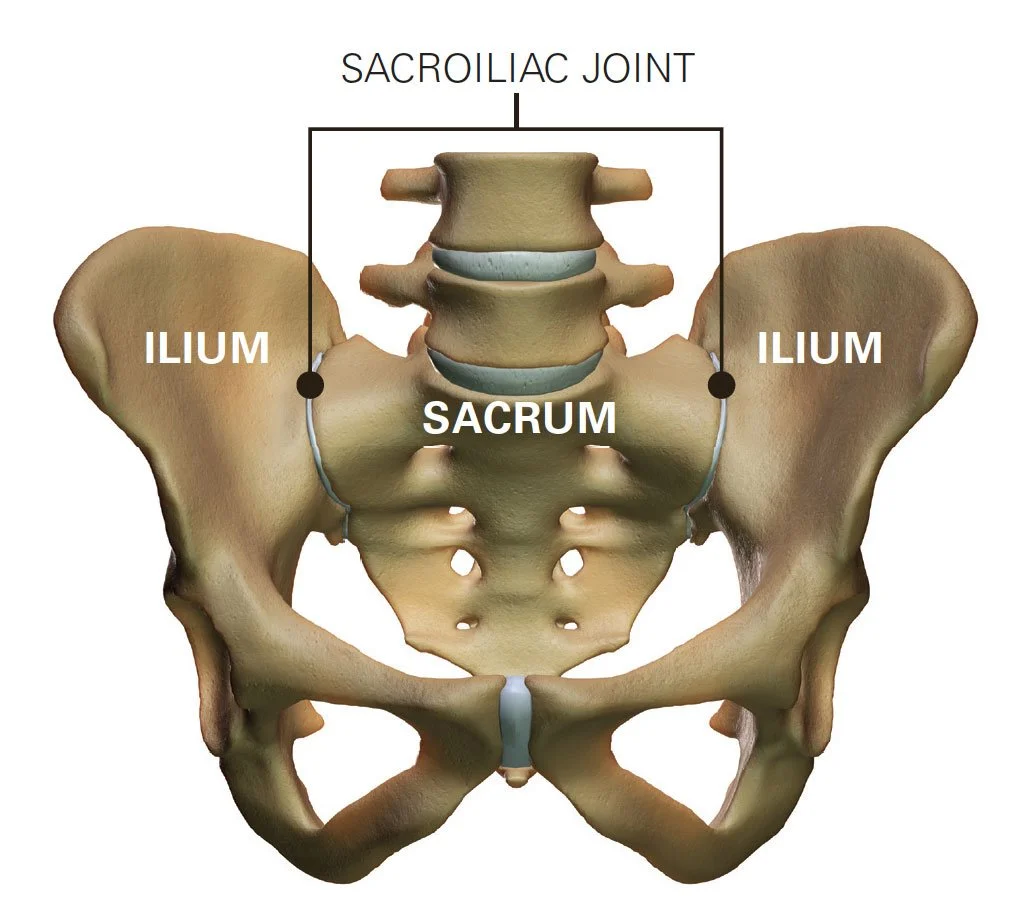
The sacroiliac joint, often abbreviated as SI joint, is a joint in the pelvis that connects the sacrum (the triangular bone at the base of the spine) to the ilium (one of the bones of the pelvis). It plays a crucial role in transferring the weight of the upper body to the pelvis and legs.
The SI joint is unique because it has limited mobility compared to other joints in the body. Its primary function is to provide stability to the spine and pelvis, rather than allowing for a wide range of motion. However, even though it has limited mobility, the SI joint can still be a source of pain and discomfort for some individuals, often due to conditions like inflammation, injury, or arthritis.
Issues with the sacroiliac joint can cause lower back pain, hip pain, and even radiating pain down the legs. Diagnosis and treatment of SI joint problems may involve physical therapy, pain medication, injections, or in some cases, surgical intervention. If you're experiencing pain or discomfort in this area, it's advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
While it is not as extensively studied as more common musculoskeletal conditions, here are some general points about the epidemiology of SI joint dysfunction:
1. Prevalence: SI joint dysfunction is relatively common but can be challenging to diagnose accurately. The prevalence of SI joint dysfunction varies in different populations, but it is estimated to affect approximately 15-30% of patients with chronic lower back pain.
2. Age and Gender: SI joint dysfunction can affect individuals of all ages, but it is more commonly seen in adults. It does not appear to have a strong gender predilection, meaning it can affect both men and women.
3. Underdiagnosis: SI joint dysfunction is often underdiagnosed because its symptoms can be similar to other musculoskeletal or spinal conditions. This can make it challenging to determine the exact prevalence in the general population.
4. Causes: The causes of SI joint dysfunction can vary and may include trauma, pregnancy-related changes, inflammatory conditions, and degenerative processes. In some cases, the exact cause may not be easily identified.
5. Comorbidities: SI joint dysfunction may be associated with other musculoskeletal conditions, such as lumbar spine issues or hip problems, which can further complicate diagnosis and treatment.
6. Diagnostic Challenges: Accurate diagnosis of SI joint dysfunction can be challenging, and it often involves a combination of clinical evaluation, medical history, imaging studies (e.g., X-rays, MRI, or CT scans), and diagnostic injections. Some patients may undergo multiple tests and evaluations before a definitive diagnosis is made.
7. Management: The management of SI joint dysfunction can include conservative treatments such as physical therapy, pain medications, and injections of corticosteroids or local anesthetics. In some cases, surgical procedures, such as SI joint fusion, may be considered for patients who do not respond to conservative treatments.
It's important to note that the epidemiological data related to SI joint dysfunction is continually evolving as medical understanding and diagnostic techniques improve.
When a physical therapist examines the sacroiliac joint (SI joint) for dysfunction or pain, they typically follow a systematic approach to evaluate the patient's condition. The examination aims to assess the joint's mobility, stability, and the presence of any related musculoskeletal issues. Here are some of the common steps involved in a physical therapist's examination of the SI joint:
Medical History: The physical therapist will start by taking a detailed medical history. They will ask questions about your symptoms, any previous injuries, surgeries, or medical conditions that might be relevant. This information helps them better understand your specific situation.
Subjective Assessment: You will be asked to describe your symptoms, including the location, intensity, duration, and any activities or positions that exacerbate or alleviate your pain. This information helps the physical therapist in forming an initial hypothesis.
Physical Examination:
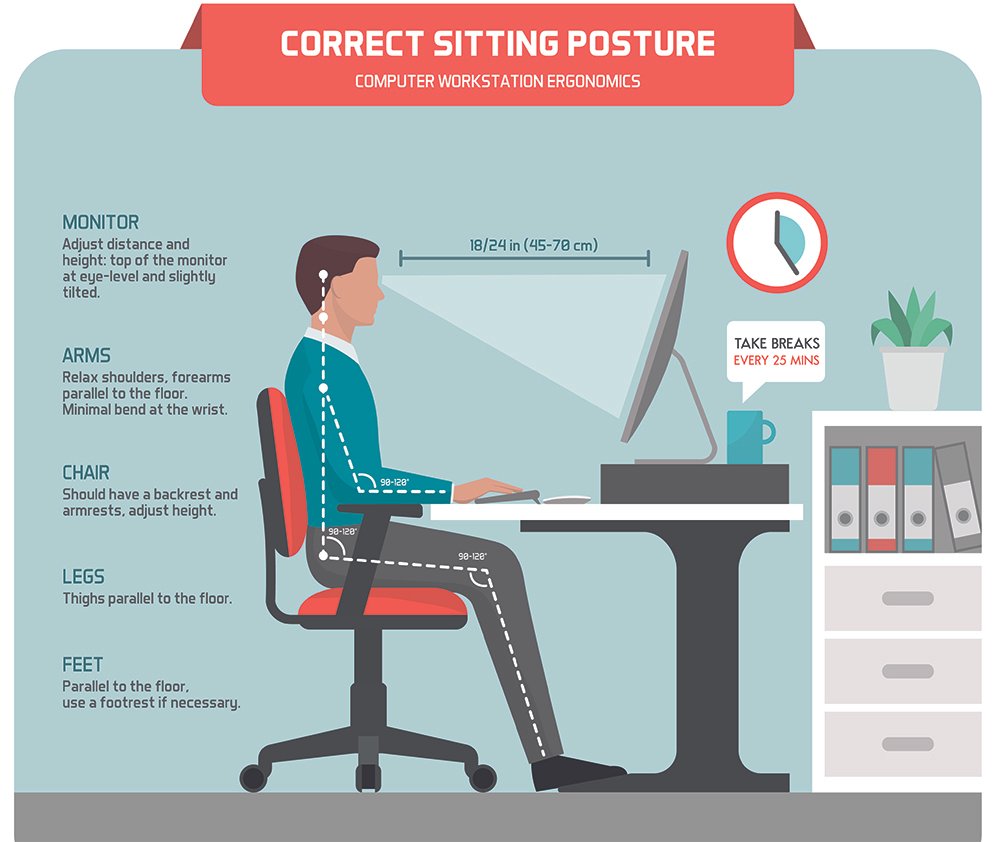
Observation: The therapist may observe your posture, gait (walking pattern), and any visible signs of muscle imbalances or joint asymmetry.
Palpation: The physical therapist may use their hands to palpate (touch and feel) the area around the SI joint, looking for tenderness, swelling, or muscle tightness.
Range of Motion: They will assess the range of motion of the lumbar spine and hips, as restrictions or limitations can contribute to SI joint issues.
Special Tests: Physical therapists may perform specific orthopedic tests to help diagnose SI joint dysfunction. These tests may include:
Gaenslen's Test
Thigh Thrust Test
Compression Test
Distraction Test
Sacral Thrust Test
Fortin Finger Test
SI Joint Compression Test
Functional Assessment: The therapist may assess your functional abilities, including activities such as walking, standing, sitting, and bending. They will look for movements or positions that reproduce your pain.
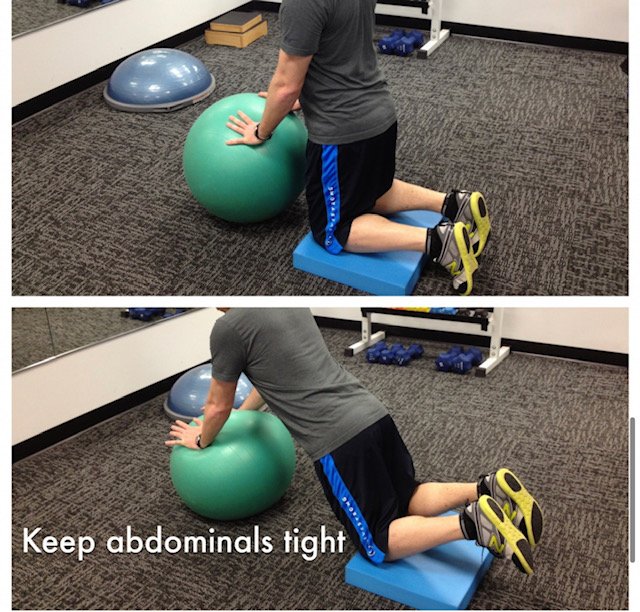
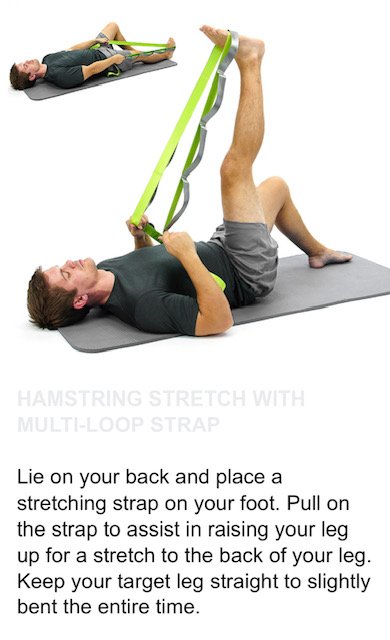
Muscle Testing: Evaluation of the strength and flexibility of the muscles surrounding the SI joint is important. Weak or imbalanced muscles can contribute to SI joint dysfunction.
Neurological Assessment: The therapist may check for any neurological symptoms or signs related to the SI joint, such as sensory changes or reflex abnormalities.
Radiological and Imaging Studies: In most cases, the physical therapist review results of X-rays, MRI, or other imaging studies to correlate with their clinical examination.
Surface palpation of the sacroiliac joint (SI joint) can be a useful component of the diagnostic process, but its reliability in isolation is limited. Palpation involves manually examining the area around the SI joint for tenderness, swelling, or other signs of discomfort. While it can provide valuable information, several factors can affect its reliability:
--Variability among Individuals: SI joint anatomy and the location of pain or discomfort can vary from person to person. Some individuals may have naturally tender or sensitive areas around the SI joint, making palpation more subjective.
--Patient Tolerance: The reliability of surface palpation can also depend on the patient's pain tolerance. Some individuals may be more sensitive to pressure, while others may not feel tenderness even when there is an issue with the SI joint.
--Surrounding Musculature: Muscles and soft tissues surrounding the SI joint can also affect the reliability of palpation. Muscle tension or trigger points in the area may cause discomfort that is not directly related to the SI joint itself.
--Experience of the Examiner: The reliability of palpation can be influenced by the skill and experience of the healthcare provider conducting the examination. A trained and experienced clinician may be more adept at identifying subtle signs of SI joint dysfunction.
--Diagnostic Support: Palpation is often used in conjunction with other diagnostic methods, such as orthopedic tests, imaging studies, and medical history. These additional tools can help confirm the findings from surface palpation.
--Differential Diagnosis: Lower back and hip pain can have various causes, including issues with the lumbar spine, hip joint, and muscles. It can be challenging to attribute pain solely to the SI joint based on palpation alone.
Given these factors, surface palpation of the SI joint is typically considered a part of the overall diagnostic process, but not the sole determinant of SI joint dysfunction. In summary, while surface palpation of bony landmarks is a part of the diagnostic process for SI joint dysfunction, it is typically not considered a standalone or highly reliable method for diagnosis.
The clinicians at Lanier Therapy in Motion use a combination of clinical assessment, orthopedic tests, imaging studies (such as X-rays or MRI), and the patient's history to arrive at a more accurate diagnosis.
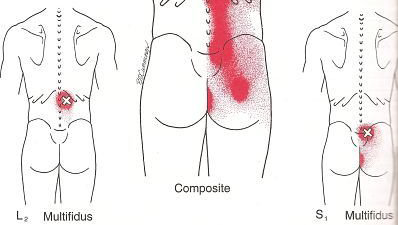
In addition, our clinicians will check for the presence of trigger points in the lower back and sacroiliac joint musculature. While trigger points themselves do not directly cause sacroiliac joint dysfunction, they can contribute to or exacerbate pain in the lower back, including the region around the sacroiliac joint (SI joint). Here's how trigger points can be related to SI joint dysfunction:
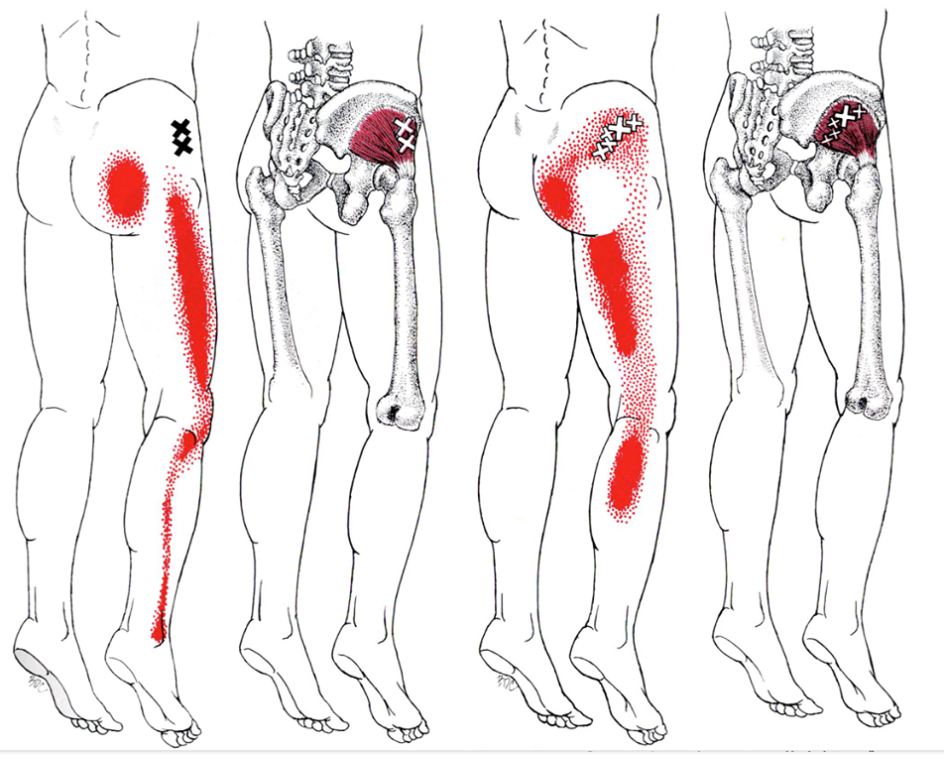
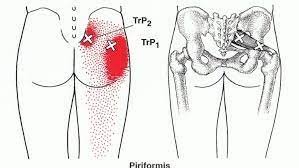
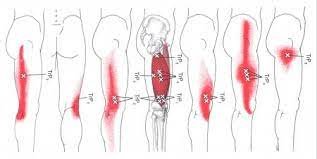
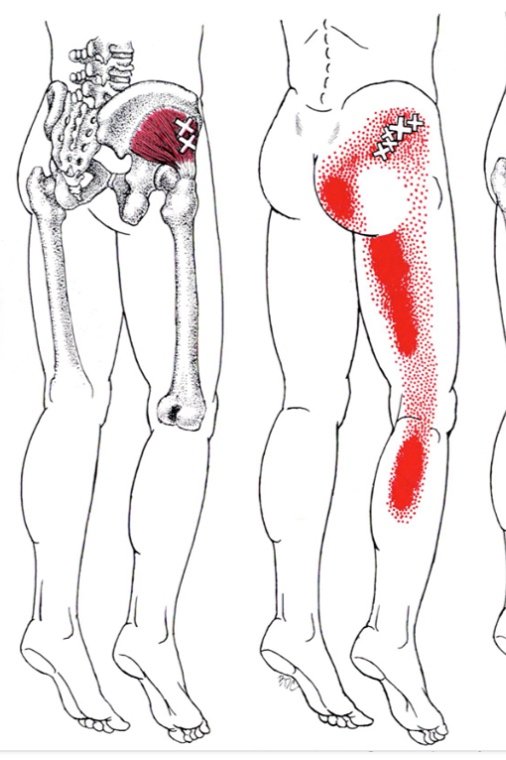
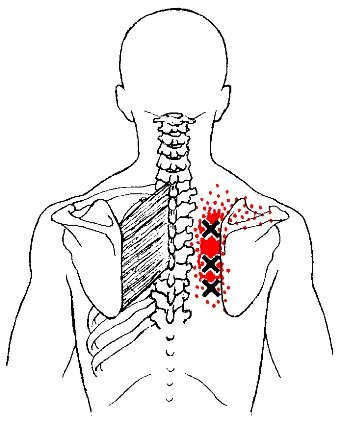
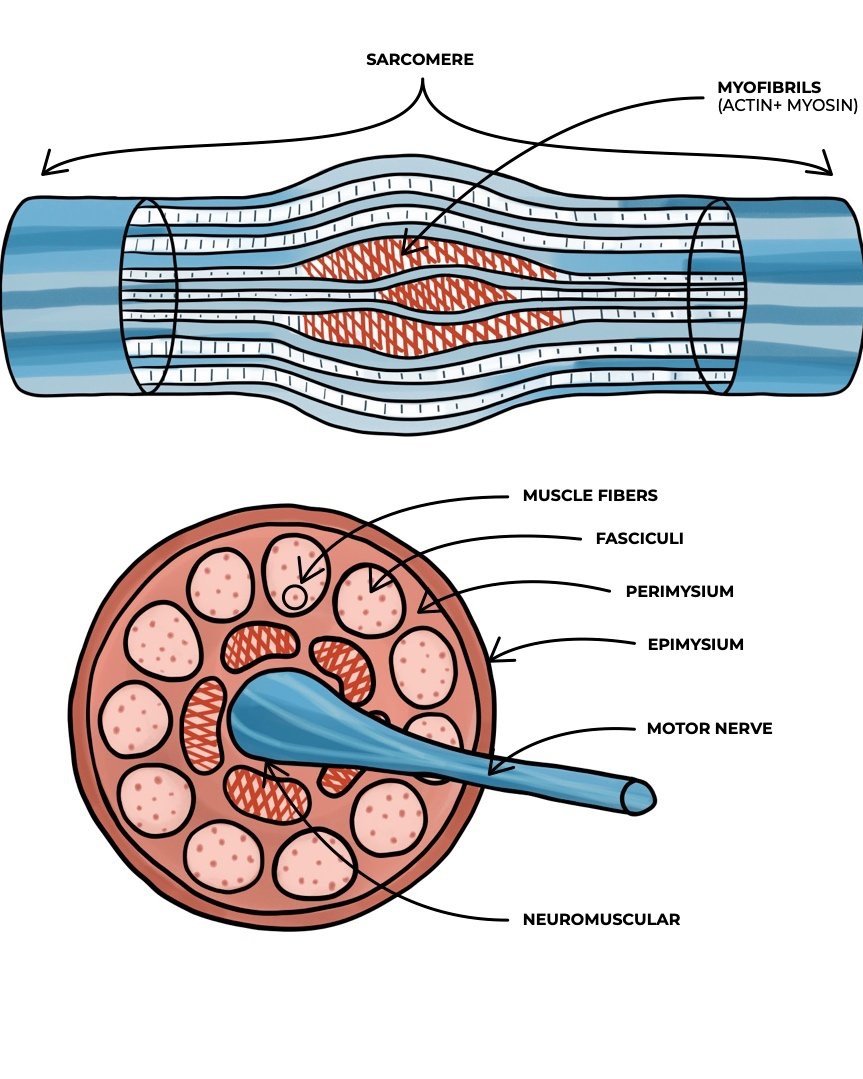
1. Muscular Imbalances: Trigger points in muscles surrounding the SI joint, such as the piriformis, gluteus medius, or erector spinae muscles, can lead to muscular imbalances. When these muscles develop trigger points, they may become tight, weak, or painful, affecting the stability and function of the SI joint.
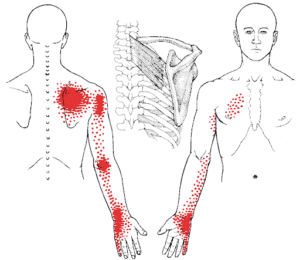
2. Referral Pain: Trigger points can refer pain to other areas of the body, meaning that the pain is felt in a location distant from the trigger point itself. Trigger points in the muscles around the SI joint can refer pain to the lower back, buttocks, or even the hip, mimicking the symptoms of SI joint dysfunction.
3. Altered Biomechanics: Muscular imbalances and trigger points can alter the biomechanics of the pelvis and lumbar spine, potentially placing additional stress on the SI joint. Over time, this altered biomechanics can contribute to SI joint dysfunction or exacerbate existing issues.
4. Pain Amplification: Trigger points can sensitize the surrounding tissues and nervous system, making them more prone to pain and discomfort. This heightened sensitivity can make it more challenging for individuals with SI joint dysfunction to manage their pain effectively.
It's essential to note that trigger points are just one potential contributor to lower back and SI joint pain. SI joint dysfunction can have various causes, including trauma, inflammation, pregnancy-related changes, or degenerative processes. Addressing trigger points, if present, can be part of a comprehensive treatment plan to alleviate pain and improve function in individuals with SI joint issues.
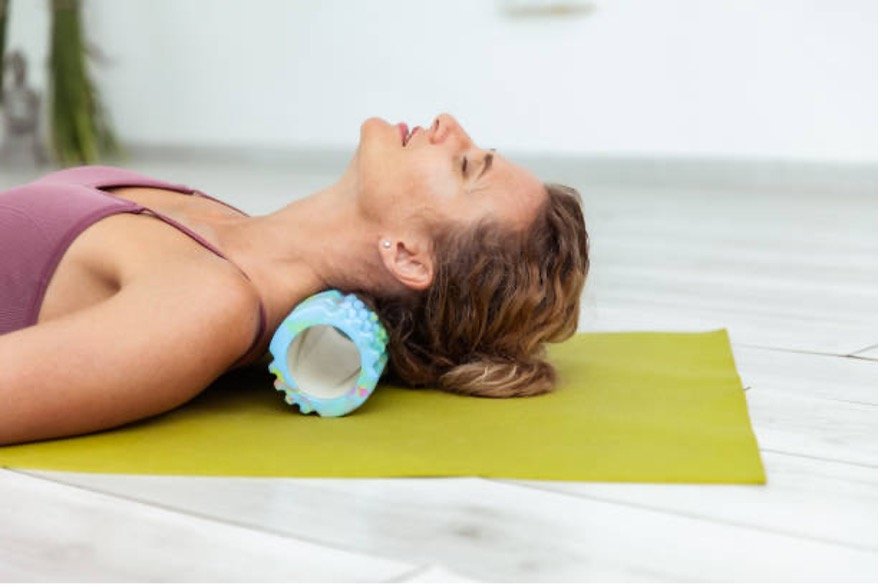
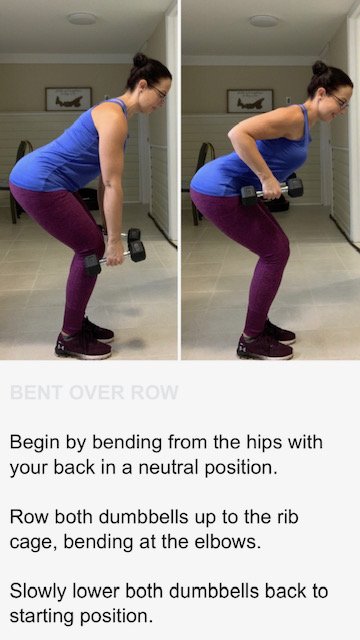
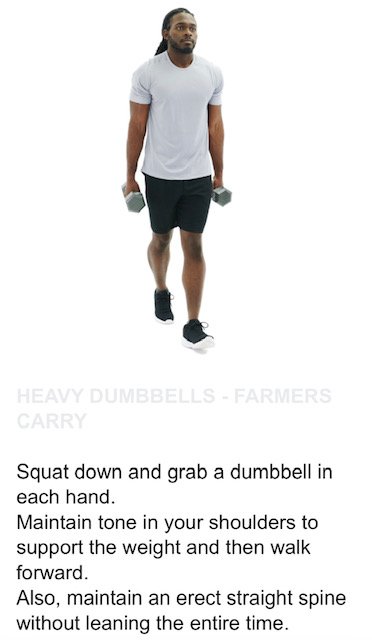
After a thorough examination, the physical therapist will discuss their findings and work with you to develop an individualized treatment plan. Treatment may include exercises to improve SI joint stability, manual therapy techniques, pain management strategies, and education on posture and body mechanics. The goal is to alleviate pain, improve function, and prevent future SI joint issues.
If you feel your pain may be related to a sacroiliac joint problem and would like to learn how to treat it successfully without surgery, please take advantage of a free consult at Lanier Therapy in Motion.